The Relevance of Culture and Cultural Sensitivity in Autism, Intellectual Disability and Behavioural Assessments and Interventions in Nigeria
Cultural sensitivity must be prioritized in autism, intellectual disability, and behavioural assessments and interventions, as these carry crucial responsibilities – foremost among them ensuring equitable and respectful care for all individuals. In the African context, cultural sensitivity is extremely important due to the interplay of deep-seated factors, where diverse cultures, traditions, and social norms shape perceptions of neurodevelopmental disorders such as autism, along with intellectual and developmental disabilities (IDD). In other words, cultural sensitivity – the concept of understanding, respecting, and appropriately responding to the relevant cultural context of individuals – is vital within assessment and intervention frameworks. Indeed, Nigeria is no exception, as these cultures greatly influence how families perceive and access behavioural services.
This article aims to highlight the issue of neurodevelopmental disorders in Nigeria, focusing on culturally sensitive approaches and emphasising frameworks that culturally acknowledge local beliefs and values.
Culture holds significant importance in both social and individual contexts, leading to profound effects on others’ beliefs, values, and behaviours. Each of us communicates and responds to the world differently based on our diverse cultural backgrounds. Addressing the cultural context of children or individuals with autism, as an ethical consideration, is essential for effective treatment. Simultaneously, professionals must recognise the impacts that culture invariably has and be aware of their own biases when conducting assessments, diagnoses, and designing behaviour change programmes. This self-awareness is a crucial aspect of our work, as it enables us to provide the best possible care. We will review how attending to cultural diversity can make interventions more ethical and practical, emphasising the role of cultural sensitivity in formulating treatment plans. For parents, technicians, caregivers, clinicians, and teachers, understanding the influence of culture is vital in supporting children and individuals with autism.
Understanding Culture in Nigeria

Nigeria boasts a rich and diverse culture, comprising over 300 ethnic groups, each with distinct languages, customs, and perspectives on life. This cultural multiplicity shapes the perceptions that individuals and families hold regarding disability and mental health issues. Many Nigerian cultures tend to conceptualise autism or IDD within spiritual frameworks, viewing them as the outcome of supernatural influences, ancestral problems, or communal issues (Ennis-Cole et al., 2013). These attitudes often normalise discrimination and stigmatisation, rendering access to professional services extremely difficult, which underscores the importance of cultural sensitivity in evaluation and intervention procedures.
The Influence of Religion and Spirituality
Religion is a fundamental aspect of Nigerian culture, primarily characterised by Christianity and Islam. Some families may interpret neurodevelopmental disorders differently, viewing them as a test from God or as a consequence of spiritual warfare. This perspective can influence how families approach diagnoses and recommendations for intervention. Although these beliefs can be complex, professionals must navigate these frameworks with great sensitivity, integrating spiritual care alongside evidence-based services. This may involve engaging in respectful discussions with families about the potential advantages of evidence-based interventions while also acknowledging and respecting their cultural beliefs.
Socioeconomic Factors
Socioeconomic status also influences cultural perceptions of neurodevelopmental disorders. Families from lower socioeconomic backgrounds may have limited access to healthcare resources, leading to a reliance on traditional healers or community support systems. Understanding these socioeconomic dynamics is crucial for practitioners to develop suitable interventions that address both the clinical and contextual needs of families (Bhatti-Sinclair, 2023). In urban areas, families may have better access to intervention services; however, stigma and misinformation can still hinder their willingness to seek help. In contrast, rural families may face greater barriers, including transportation issues and a lack of trained professionals. Addressing these disparities is essential for creating equitable access to behavioural services across Nigeria.
The Role of Cultural Sensitivity in Assessment and Diagnosis
1. Perception and Interpretation of Behaviours
Cultural bias and behavioural evaluation are two facets of the same phenomenon, as a lack of cultural sensitivity can hinder practitioners from understanding behaviours within cultural contexts. For instance, behaviours perceived as bizarre in Western settings may be interpreted differently by Nigerians due to significant value differences in communal culture and social norms. Tafla et al. (2024) explained how a lack of understanding of different cultures can lead to misdiagnoses and ineffective treatment strategies.
For example, a withdrawn child may be seen as disengaged and interpreted as being shy in some cultures. In contrast, in others, this behaviour may be attributed to a lack of proper cultural understanding. Without adequate cultural insight, such an individual may be labelled as having a developmental disorder. Various cultures offer different perspectives; therefore, practitioners bear the responsibility of employing suitable culturally responsive frameworks to achieve the desired outcomes, avoid misdiagnosis, and provide the correct support.
2. Engagement with Families
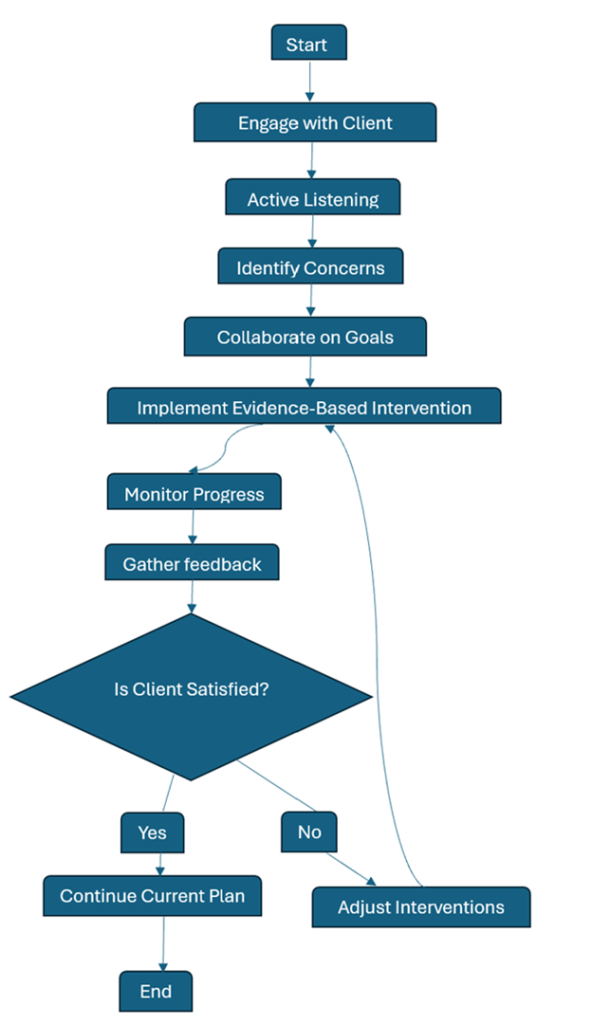
By involving families in the assessment process, practitioners can build trust and rapport, which are essential for achieving successful outcomes. This approach not only ensures that the proposed intervention is acceptable to the family but also respects their cultural values and beliefs. The outcome is a more effective and ethical intervention, leading to improved patient outcomes and increased trust in healthcare professionals.
It is advisable to consider family meetings where practitioners invite relevant family members to share their opinions and concerns. In doing so, practitioners can build essential rapport and trust, which are crucial for achieving successful outcomes. Furthermore, including other relatives such as grandparents, aunts, and uncles can provide additional avenues of support that may enhance the overall assessment.
3. Communication Styles
Communication in Nigeria tends to be indirect and relies heavily on context due to a culture that emphasises respect and hierarchical structures. Families must be listened to attentively so that practitioners can grasp the essence of what is being communicated. In this regard, individuals with whom practitioners engage need to feel valued, which extends beyond vocal communication. Practitioners must be mindful of non-vocal cues and the significance of relational dynamics in discussions about assessments and behaviour (Iqbal, 2021).
For instance, conducting assessments in indigenous languages or dialects can enhance understanding and foster comfort. Additionally, practitioners must consider how they frame, pose, and respond to questions, ensuring that the language used is respectful and appropriate. Employing narrative frameworks to articulate ideas facilitates effective communication, as they align with traditional Nigerian practices and convey profound, intricate ideas or concepts in a relatable manner.
Culturally Sensitive Interventions
1. Tailored interventions
Intervention implementation should consider the culture and society of Nigerian families. Such interventions should take into account the community’s social customs, income levels, and available resources. Culturally appropriate interventions that incorporate local languages, terminology, and materials are likely to encourage family participation and improve outcomes (Smith, 2020).
Tailoring strategies may involve adapting intervention approaches to align with local culture. For example, utilising storytelling or social activities can enhance relatability for children with neurodevelopmental disorders. Additionally, community leaders can be incorporated into the practitioner’s intervention to improve acceptance and foster respect.
2. Training for Practitioners
Training programmes for healthcare professionals should integrate the culture of the populations they serve. Strategies involve purposefully examining local culture and engaging in reflective practices. This also includes the development of culturally complex skills. Culturally sensitive professional development training has the potential to enhance the efficacy of assessment and intervention (Gorden, 2023).
Specific primary and secondary instructional techniques, including community education and outreach to promote neurodevelopmental disorders and services, need to be established. These strategies encourage active participation from families and the community. Professionals should organise workshops and seminars on cultural sensitivity to promote the sharing of practitioners’ experiences and peer learning.
Challenges and Opportunities
1. Stigma and Misunderstanding
Cultural stigma continues to persist in Nigerian society regarding neurodevelopmental disorders, despite heightened awareness. Many families fear social stigma or discrimination and are thus hesitant to seek help. To promote acceptance and understanding, it is vital to change this outlook through education and community advocacy (Lichtensztejn et al., 2024).
Prominent community figures and leaders can assist in shifting perceptions of neurodevelopmental disorders and encouraging families to seek support without fear of stigma through positive narratives. Awareness campaigns, public forums, and support groups contribute to eliminating the stigma surrounding these disorders, fostering a more accepting environment for affected individuals and their families.
2. Resource Limitations
Assessments and interventions that are culturally sensitive can be challenging to deliver. The lack of resources and trained professionals makes it exceedingly difficult to obtain culturally appropriate assessments and interventions. Collaboration among government branches, NGOs, and community groups is essential for increasing the availability of services and improving their accessibility (Griffith et al., 2024).
Investing in training local residents and developing community-based services can help alleviate these resource-related challenges. Furthermore, using technology, such as telehealth, can enhance the delivery of intervention services to remote and underserved areas.
3. Policy and Advocacy
Culturally sensitive practices, particularly those concerning neurodevelopmental disorders, require advocacy for care policy. Public and private funding priorities ought to concentrate on training, community outreach, and pertinent research, which are measurable efforts. Nigeria can improve the quality of care for individuals with neurodevelopmental disorders, thereby fostering an environment that values cultural sensitivity.
Efforts should also concentrate on developing national guidelines that integrate cultural considerations into intervention practices, ensuring that all professionals are prepared to deliver culturally competent care. Collaboration with other African organisations can further enhance these initiatives by offering additional resources and expertise.
Conclusion
Cultural sensitivity is not merely an ethical imperative; it is a practical necessity within the realm of behavioural assessments and interventions for neurodevelopmental disorders in Nigeria. By recognising and respecting the cultural beliefs and practices of families, practitioners can foster improved engagement, enhance outcomes, and ultimately contribute to the well-being of individuals with autism and intellectual and developmental disabilities (IDD). As the field continues to evolve, ongoing dialogue and collaboration among stakeholders will be essential in creating culturally informed practices that resonate with the diverse populations they serve.
The journey towards culturally sensitive behavioural care in Nigeria requires commitment from all stakeholders, including healthcare providers, families, community leaders, and policymakers. By collaborating, they can create a more inclusive and supportive environment that acknowledges the unique cultural contexts of individuals and families affected by neurodevelopmental disorders.
Reference
Bhatti-Sinclair, K. (2023). Culturally appropriate interventions. In Cultural Competence in Social Work Practice.
Ennis-Cole, D., Durodoye, B. A., & Harris, H. L. (2013). The impact of culture on autism diagnosis and treatment: Considerations for counselors and other professionals. The Family Journal: Counseling and Therapy for Couples and Families, 21(3), 279-287.
Gorden, N. (2023). The role of culture and diversity in ABA treatment plans: Creating culturally sensitive and ethical interventions. Different Roads to Learning Blog.
Griffith, D. M., Efird, C. R., Baskin, M. L., Webb Hooper, M., Davis, R. E., & Resnicow, K. (2024). Cultural sensitivity and cultural tailoring: Lessons learned and refinements after two decades of incorporating culture in health communication research. Annual Review of Public Health, 45, 195-212.
Iqbal, T. (2021). Importance of intercultural sensitivity. MAP Education and Humanities, 1(2), 1-6.
Lichtensztejn Tafla, T., Triguero Veloz Teixeira, M. C., Woodcock, K. A., & Sowden-Carvalho, S. (2024). Autism spectrum disorder diagnosis across cultures: Are diagnoses equivalent? Journal of Autism and Developmental Disorders.
Smith, J. D. (2020). Introduction to cultural considerations in collaborative and intervention assessment. Journal of Personality Assessment, 98(6), 563-566.
Tafla, T. L., Triguero Veloz Teixeira, M. C., Woodcock, K. A., & Sowden-Carvalho, S. (2024). Autism spectrum disorder diagnosis across cultures: Are diagnoses equivalent? Journal of Autism and Developmental Disorders.